
Outpatient Observation Management – Impact on Financial Cost & Best Practices
Placing a patient in the most appropriate level of care is important to ensure the patient is cared for with the right level of services and the hospital is reimbursed appropriately for services rendered. However, many hospitals are challenged by the status determination process, and often over utilize the observation level of care. According to publicly available Medicare data, the national average observation rate (the ratio of bedded observation to inpatient cases) was 18% in 2019. The state average observation rate for Illinois facilities in the same period was 25%. This means that most short-term acute care facilities in Illinois had an observation rate that exceeded the national average (Figure 1). There are considerable financial implications to patient discharge status, which often results in missed revenue. Hospitals and health systems should consider implementing status determination process improvements to augment net patient revenue while prioritizing patient outcomes.
Figure 1: Traditional Medicare Observation Rates for Illinois short term acute care facilities
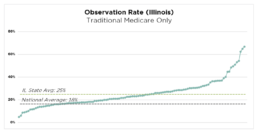
Source: Publicly available Medicare data. Represents Traditional Medicare only.
Observation Status and Medical Necessity
Observation status is an outpatient designation that allows providers to place a patient in an acute care setting to monitor the need for an inpatient admission. Common signs and symptoms including chest pain, shortness of breath, nausea/vomiting/stomach pain and fever might result in placement in observation for further testing. Appropriate observation patients typically have much lower acuity and severity of illness compared to inpatient level of care, and are commonly discharged from the facility in observation status within 24-36 hours.
A bedded observation patient can also be appropriately converted to inpatient status if there is evidence of medically necessary care. “Medical necessity”, the principle defined by CMS and other payors, establishes the distinction and substantiating evidence between observation and inpatient levels of care. Medical necessity is documented within the medical record, and should clearly and precisely illustrate the complexity of medical factors and the reasoning for the required inpatient admission (Figure 2). Inadequate documentation can result in payor denial for inpatient authorization and refusal of payment for services delivered. Physician documentation is the cornerstone for appropriate status determination, and there can be significant financial implications to the chosen level of care.
Figure 2: Example of How Appropriate Medical Necessity Documentation Can Support an Inpatient Admission
Observation Appropriate
- Patient complaint of shortness of breath
- Abnormal labs
- Vital signs stable
- Will need to monitor
- Consult Nephrology and cardiology
Inpatient Appropriate
- Patient complaint of shortness of breath with imaging findings of new onset of congested heart failure
- Lasix 80mg IV given
- Oxygen saturation 87% on room air, improved to 100% ounce on 4L ofO2
- Abnormal renal function consider, acute kidney injury
- Will need cardiology and nephrology consulted
- Patient appropriate for inpatient level of care anticipate 2 midnight stay
Financial Implications of Observation Management
Delivery of care and outcomes are the priority. But appropriate patient status and level of care determination can significantly affect net revenue. Payor reimbursement (for both government and private payors) typically differs considerably between observation and inpatient status. While the nuances of payor agreements may vary across payors and facilities, reimbursements for observation discharges are often lower than inpatient payments While this reimbursement differential can vary, a typical Traditional Medicare case can provide an illustrative example. CMS IPPS and OPPS final rules stipulates that a standard inpatient case is reimbursed approximately $6,500, while a standard observation discharge is reimbursed approximately $2,000. In this example, there is approximately a $4,500 reimbursement variance for a case that might have received the exact same care, but was discharged in an inappropriate status. This positive reimbursement variance is similarly prevalent with other government and private payors. Across most payors, documentation of medical necessity and deliberate processes for status determination can have a significant impact on net patient revenue.
Appropriate patient status determination and discharge status can also have significant financial implications for the patient. A discharge from observation status may result in a higher out-of-pocket expense to the patient compared to an inpatient discharge. Since observation status is an outpatient service, a Medicare patient pays 20% of billed charges for coinsurance.
Observation Management Best Practices
There are several ways that a facility can align care delivery and revenue cycle functions through level of care and status determination processes.
Care Team Collaboration
Collaboration and communication among the care team members (providers, utilization management, and nursing staff) is critical to a successful observation management program. This includes deliberate discussions regarding patient needs and plan of care between care teams. This also includes documentation within the medical record that clearly substantiates the medical necessity. A dedicated huddle to focus on observation patients also enables communication and collaboration. This observation huddle serves as a forum for Case Management, Utilization Management and Physician Advisors to review all observation patients at least once per day and is an effective method to highlight any barriers to discharge, necessary follow-up actions, and status conversion potential.
Status Determination at the Portal of Entry
Appropriate status determination from the Emergency Department reduces the need for conversion to an inpatient status later in the stay and helps place the patient in an appropriate care setting. Facilities with leading patient status processes dedicate Case Management/Utilization Management staff in the emergency department to own the initial status determination process. These staff should be integrated into a collaborative process between ED providers and hospitalists that focuses on effective communication, accurate initial medical necessity reviews, and timely provider documentation of patient needs and acuity.
Utilization of Observation Units
When observation cases are bedded on inpatient units, care teams often have difficulty differentiating between patients placed in observation status or inpatient status. This results in longer lengths of stay for observation cases, and increased resource utilization for observation care. A hospital can delineate patient status assignments by implementing a unit focused exclusively on observation patients. Sometimes these units are within or adjacent to emergency departments. This enables the care team to automatically differentiate observation patients from other bedded patients. It also allows for increased monitoring of observation patients (recommended rounding 3x per day vs 1x per day). Sometimes facilities will introduce diagnosis-specific algorithms to aid in this colocation process, including chief complaints such as chest pain, syncope and collapse, heart disease, cellulitis, and headaches. If a dedicated observation unit is not possible, providers and transfer centers should attempt to cohort observation patients as much as possible.
Physician Advisor Integration
A sophisticated Physician Advisor (PA) program utilizes the PA resource as an engaging liaison between Case Management, Utilization Management, providers, and administration. The PA can aid in the status determination process through secondary review of the observation cases, and can assist the UM team and providers through the documentation process. The PA may also be involved in additional processes including payor appeals, denials management, education for providers, and other quality improvement efforts.
